Key Takeaways
- Alcohol can lower or raise blood sugar—and sometimes both. Sugary drinks can cause an initial spike, while alcohol itself can lead to delayed drops in blood sugar hours later.
- Low blood sugar is the biggest risk, particularly if you drink on an empty stomach or have diabetes and take insulin or certain medications.
- If you do drink alcohol, eat before drinking, choose lower-sugar beverages, stay hydrated, and monitor blood sugar for up to 24 hours after drinking, especially before bed.
Alcohol can make blood sugar go up, down, or both during the same drinking session. These changes occur because alcohol affects how your body manages glucose (sugar). The effects depend on what you drink, how much you consume, and whether you’ve eaten.
How Alcohol Lowers Blood Sugar Levels
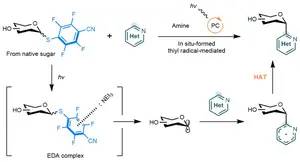
Alcohol lowers your blood sugar by limiting your liver’s ability to release glucose. This effect can be delayed, meaning blood sugar may drop hours after drinking rather than right away.
Your liver helps keep your blood sugar steady by storing glucose and releasing it when your body needs energy. When you drink alcohol, your liver sees it as a toxin and prioritizes breaking it down first, and releases less glucose.
Even without diabetes, you can experience drops in blood sugar, especially when drinking alcohol.
Warning Signs of Low Blood Sugar
Low blood sugar (hypoglycemia) from drinking is dangerous because symptoms mimic being drunk, making it hard to recognize medical distress. Common warning signs include:
- Blurred vision
- Confusion or unclear thinking
- Dizziness
- Fast heartbeat
- Fatigue
- Headache
- Hunger
- Irritability
- Shakiness
- Sweating
Who Is Most at Risk?
Your risk of experiencing blood sugar drops from drinking increases when you:
- Have diabetes: Low blood sugar is more common among those with diabetes.
- Drink heavily: Higher alcohol intake keeps your liver focused on processing alcohol instead of supporting blood sugar balance.
- Drink on an empty stomach: Food slows how quickly alcohol enters your bloodstream and provides glucose your body can use.
- Exercise before or after drinking: Especially in those with diabetes or who take insulin.
How Alcohol Can Raise Blood Sugar
Alcohol is better known for lowering blood sugar, but it can also raise it. A blood sugar crash can also follow the spike several hours later. Blood sugar spikes are more common when you:
- Are dehydrated (this increases glucose concentration in your blood)
- Choose drinks with high sugar or carbohydrates
- Drink large portions quickly
- Have insulin resistance or diabetes
Some drinks and mixers increase your risk of this spike because they are high in sugar and carbohydrates. Examples include:
- Flavored syrups
- Frozen cocktails
- Juice or soda
- Regular beer
- Cocktail mixes
- Sweet liqueurs or wines
- Tonic water
Lower-risk alcoholic drinks and mixers with less sugar and carbs include:
- Diet tonic water
- Distilled spirits (vodka, whiskey, tequila)
- Dry wine
- Light or low-carbohydrate beer
How Long Alcohol Can Affect Blood Sugar
Alcohol’s impact on blood sugar doesn’t stop when your last drink does. Changes can continue for many hours afterward.
Overnight Blood Sugar Changes
The most dangerous drops typically happen six to 12 hours after your last drink. Your liver is still processing alcohol and cannot make new glucose to keep your levels stable.
The highest risk often occurs while you’re sleeping because you’re less likely to notice hypoglycemia symptoms while you’re asleep as your sugar continues to drop.
Can Alcohol Affect Blood Sugar the Next Day?
Alcohol can affect blood sugar for up to 24 hours. This is especially true for those with:
Even if you feel fine, blood sugar levels may still be harder to control the next day.
Long-Term Effects of Alcohol on Blood Sugar and Insulin
Drinking alcohol once in a while may only affect your blood sugar for a short time. But drinking often or in large amounts, more than one drink a day for women or more than two drinks a day for men, can cause longer-term problems.
Long-term alcohol use can damage your:
- Endocrine system: Controls hormones that help manage blood sugar and metabolism
- Liver: Stores and releases sugar when your body needs energy
- Pancreas: Makes insulin, which helps move sugar from your blood into your cells
When chronic alcohol use causes damage or inflammation to these organs or systems, your blood sugar becomes harder to control. Insulin resistance can develop, meaning your body does not respond to insulin as well as it should. As a result, blood sugar levels may stay high, increasing the risk of type 2 diabetes.
How to Drink Alcohol More Safely If You’re Managing Blood Sugar
You can help lower your risk of alcohol-related blood sugar drops by:
- Eating a meal with protein and complex carbohydrates
- Limiting yourself to one drink per hour
- Alternating alcohol with water
- Checking your blood sugar before bed after drinking (to catch delayed drops)
If your blood sugar drops below 70 milligrams per deciliter (mg/dL):
- Consume fast-acting carbs (e.g., glucose tablets, 4 ounces of juice, or 1 tablespoon of honey)
- Wait 15 minutes and recheck your blood sugar
- Repeat the process if your sugar is still below 70 mg/dL
It’s best to continue monitoring your blood sugar for several hours. Avoid trying to “sleep it off,” since untreated low blood sugar can be dangerous.
Alcohol and Diabetes
If you have diabetes, alcohol creates additional risks. If you mix alcohol with diabetes medications, your risk for hypoglycemia increases. This is especially true of insulin and sulfonylureas like Glucotrol (glipizide).
Those with type 1 diabetes also face a higher risk of diabetic ketoacidosis (DKA) when drinking alcohol. People with type 2 diabetes may experience worsened insulin resistance from drinking.
Because of these serious risks, follow these safety measures if you choose to drink:
- Carry a source of sugar for emergencies.
- Check your blood sugar frequently while drinking, especially before bed.
- Do not exercise in the hours before or after drinking.
- Don’t drink alone.
- If you count carbohydrates as part of your meal plan, ask your provider how alcohol fits into your plan.
- Set an alarm to check your blood sugar overnight.
- Use a continuous glucose monitor (CGM) when available.
- Wear a medical alert ID.

:max_bytes(150000):strip_icc():format(webp)/ProfilePictureVerywell-382fc2934d094ccca87fb8df24aff298.jpg)